Home mechanical ventilation therapy
Ventilated patients have complex, evolving needs that require personalised care, and attentive management and monitoring. Learn how advanced ventilation technologies can promote effective titration, monitoring and ventilation and discover ResMed solutions that could provide a better experience for your patients.
Ventilation technologies to improve your patients’ experience
Effective ventilation systems should enhance treatment efficacy, promote comfort and reduce patient-ventilator asynchronies. ResMed offers responsive settings, modes and algorithms that are easy to set and adjust, alongside informative, user-friendly monitoring and management tools.
Key considerations when initiating home NIV
Successful ventilation therapy requires careful setup and titration. New, home-based protocols have been shown to be at least as effective1-4, can help healthcare providers to make more efficient use of limited resources.5
Before initiating home mechanical ventilation, it is important to perform a comprehensive analysis of the patient’s motivation, home situation, family support, medical history and current health status. All patients, regardless of their underlying disease, may experience symptoms of nocturnal hypoventilation such as poor sleep, frequent awakenings, headaches, fatigue and reduced alertness that should be taken into account before initiating home NIV. The potential benefits of home mechanical ventilation also vary: for example, it can significantly increase life expectancy for patients with NMD, and it can relieve symptoms and improve quality of life for those with progressive conditions like COPD.5

FAQ: the titration process
The primary aim of mechanical ventilation is to improve pulmonary gas exchange and facilitate the recovery of tired respiratory muscles by giving them sufficient rest. After a baseline assessment, mechanical ventilation is initiated with standard settings. Ventilator parameters, such as tidal volume, respiratory rate, PEEP and FiO2, are then adjusted. Patient comfort and patient-ventilator synchrony are addressed, and settings are reassessed to ensure the treatment is adapted to the patient’s needs and preferences.
Here are some questions you might ask yourself during titration.
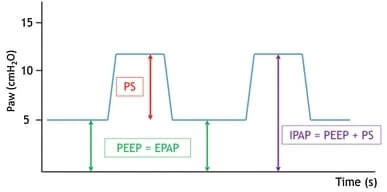
PS (Pressure Support) is the pressure difference between the IPAP (Inspiratory Positive Airway Pressure) and EPAP (Expiratory Positive Airway Pressure) that is delivered by the ventilator with each breath. PS defines how much air the patient will receive at each breath and helps to correct nocturnal alveolar hypoventilation. Some ventilators use settings like “IPAP/EPAP” or “PS/PEEP” to automatically set PS or IPAP.6
EPAP settings serve different purposes depending on the treated pathology. In patients with obstructive conditions like COPD, intrinsic PEEP is common. These patients can struggle to complete exhalation, but EPAP helps them by reducing the respiratory effort that is required to trigger a breath. In conditions like OHS, an appropriate EPAP setting can prevent upper airway collapse during sleep.
It is essential to progressively adjust EPAP while observing patient effort. If EPAP is set too low, the patient may struggle to trigger effectively, leading to delayed triggering, ineffective efforts, exhaustion and non-compliance. Conversely, if EPAP is set too high, it can lead to leaks and discomfort for the patient. 6
ResMed’s AutoEPAP algorithm automatically adjusts EPAP to maintain an open upper airway. It is available in Lumis ST, ST-A, Stellar 150 and Astral devices. Keen to learn more? Discover ResMed AutoEPAP. https://eudev-www.resmed.com/professionals/respiratory-care/niv-therapy/managing-ventilated-patient/autoepap/
A backup rate triggers the ventilator to provide support when the patient is not breathing adequately on their own. By configurating a backup rate, you can ensure that your patient will receive adequate ventilation at all times. The backup rate is usually set slightly lower than the patient’s spontaneous rate, promoting patient-triggered breaths. The lack of a backup rate is associated with an increased number of mixed and central upper-airway events in patients with obesity-hypoventilation syndrome.6
Rise time refers to the time it takes for the ventilator to transition from EPAP to IPAP. Rise time can be adjusted to reflect the patient’s ventilatory requirements, disease type and physical condition. This can help to improve their work of breathing, comfort and synchrony. Patients with high ventilatory demand, such as those with COPD, may feel more comfortable with a faster rise time; others, such as those with NMD, may prefer a slower pace. 6
All ResMed ventilators offer Rise Time, a feature that enables you to fine-tune the time required for the device to reach IPAP. Keen to learn more? Discover ResMed Rise Time and Fall Time https://eudev-www.resmed.com/professionals/respiratory-care/niv-therapy/managing-ventilated-patient/rise-fall-time/
Fall time is the time it takes for the airway pressure to transition from IPAP to EPAP when cycling occurs. Different individuals require different amounts of time to transition to exhalation. Adjusting fall time to reflect the patient’s physical needs and preferences can improve patient-device synchrony and breathing comfort, particularly for those with limited expiratory flow. It is thought that an adjustable fall time may be particularly useful for patients with advanced COPD. These patients may experience a small airway collapse on exhalation which could potentially be alleviated by a longer fall time.6
ResMed Fall Time enables you to personalise the time it takes for your patient’s device to reach EPAP. It is available in Stellar ventilators. Keen to learn more? Discover ResMed Rise Time and Fall Time https://eudev-www.resmed.com/professionals/respiratory-care/niv-therapy/managing-ventilated-patient/rise-fall-time/
The trigger, or inspiratory trigger, determines when the patient’s inspiration starts. Trigger sensitivity is a crucial parameter to ensure patient-ventilator synchrony. While a medium trigger may be suitable when the patient is awake, the sensitivity level must be adapted for sleep time to avoid ineffective inspiratory efforts. 6
ResMed’s Trigger and Cycle feature enables you to fine-tune the effort required to start and finish a breathing cycle. It is available in all ResMed ventilators. Keen to learn more? Discover ResMed trigger and cycle settings https://eudev-www.resmed.com/professionals/respiratory-care/niv-therapy/managing-ventilated-patient/trigger-and-cycle/
The cycle, or expiratory trigger, determines when the inspiration ends. As such, cycle sensitivity is a crucial parameter that underpins patient-ventilator synchrony. Ideally, the ventilator cycle should align with the patient’s natural breathing cycle. Premature cycling, where air delivery stops too quickly, and late cycling, where the ventilator keeps delivering air after the end of the patient’s breath,can both undermine the patient’s comfort. The expiratory trigger should be adjusted to achieve an inspiration time that reflects the patient’s respiratory mechanics and their obstructive or restrictive condition.6
All ResMed ventilators offer a Trigger and Cycle feature that enables you to fine-tune the effort required to start and finish a breathing cycle. Keen to learn more? Discover ResMed trigger and cycle settings https://eudev-www.resmed.com/professionals/respiratory-care/niv-therapy/managing-ventilated-patient/trigger-and-cycle/
When a patient triggers a breath and the ventilator is in pressure support (PS) mode, the inspiration time is determined by the patient’s effort and respiratory mechanics as well as by specific ventilator settings like pressure rise time, IPAP and expiratory trigger sensitivity. By setting a maximum inspiratory time (TiMax), you can limit the duration of the inhalation phase. This can be useful in situations where significant air leaks, delays in reaching the flow-cycling criterion or challenges matching the patient’s natural inhalation pace might cause the ventilator to spend too much time in the inspiratory phase. A minimum inspiratory time (TiMin) can also be set to guarantee sufficient time for inhalation, with a view to enhancing alveolar ventilation.6
ResMed TiControl sets minimum and maximum limits on inspiratory time to match the patient’s natural inspiration needs. It is featured in all ResMed ventilators. Keen to learn more? Discover ResMed TiControl https://eudev-www.resmed.com/professionals/respiratory-care/niv-therapy/managing-ventilated-patient/ticontrol/
To ensure the patient receives their prescribed pressure at the mask, the breathing circuit and patient interface should be configured and calibrated so that the ventilator can measure and offset circuit resistance. Configuring the mask type within the ventilator algorithm also makes it easier to control intentional leak and estimate unintentional leaks.6
Initiating remote care
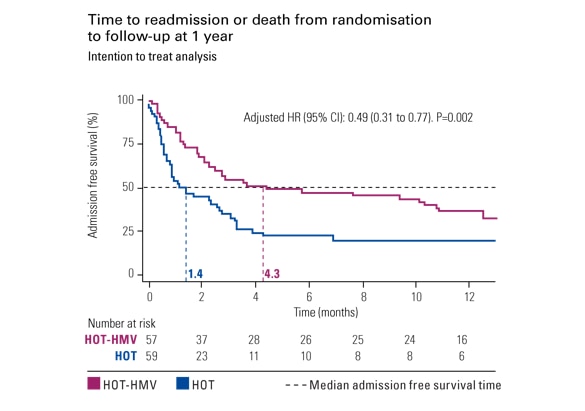
Home NIV is often initiated in hospitals. This process is costly and resource-intensive for healthcare professionals and inconvenient for patients, especially those with serious illnesses or severe disabilities, who have to travel and spend time away from home in a stressful hospital environment. Fortunately, trials have shown that initiating NIV at home for patients with neuromuscular diseases, restrictive chest diseases and COPD is as effective as hospital-based initiation and reduces costs by more than 50%.5
FAQ: Remote monitoring
Telemonitoring can be used to manage ventilated patients in a range of ways. Access to relevant data enables you to monitor and track changes in the clinical status and device parameters of individuals and groups of patients, while notifications can alert you when a patient requires attention. The ability to remotely control and adjust your patient’s device settings further facilitates efficient, timely care and helps you to support early therapy adherence and efficacy. With telemonitoring, patients have a better quality of life, fewer hospital readmissions and a reduced risk of exacerbations.7-9
Ventilators can record a range of data including usage, AHI, airway pressure, flow, tidal volume, leaks, inspiratory / expiratory times, trigger and cycle, and respiratory rate. Ventilators can record these variables with high precision and store the data on a memory card, USB stick or in the cloud. Some ventilators can automatically upload data to patient management platforms for remote monitoring.
ResMed’s AirView patient management system enables you to access, analyse and share your patient’s respiratory data with ease and track changes in your patients’ clinical condition. Keen to learn more?
If a patient starts to use their ventilator less, it may be an indication that they are struggling to tolerate their treatment, for example due to adverse effects or inadequate settings. Equally, increased ventilator use could indicate an increased need for ventilatory support, possibly due to disease progression. The patient’s total daily use of NIV is recorded in the form of statistics and trends.7
Unintentional leaks are a frequent adverse event in NIV. They affect ventilation quality and can lead to decreased compliance, patient-ventilator asynchrony, and a deterioration in sleep quality. Detailed telemonitoring data can help clinicians and home-care providers to identify and manage unintentional leaks remotely. Leak statistics and trends can be used to determine where and why a leak is occurring and enable leak resolution, which is associated with improved NIV efficiency.7 The use of ventilator data facilitates early, objective leak detection and the subsequent adaptation of parameters.7
Ventilator data can be used to examine the patient’s AHI (Apnoea-Hypopnea Index) score and their flow waveform. AHI measures the number of times that the patient’s breathing stops or is significantly reduced during every hour of sleep. AHI is a useful measurement for patients with obstructive sleep apnoea or obesity hypoventilation syndrome if there are no unintentional leaks. It may miss upper airway obstructions if leaks or laryngeal blockages are present. Examining the flow waveform can help clinicians to identify events that AHI misses. The waveform shape can suggest the cause of upper airway obstructions, though polygraphy may be needed for confirmation.
Patient-ventilator synchrony is evaluated using statistics and can be closely examined in pressure and flow waveforms. The overall synchrony is displayed along with the percentage of breaths that are triggered and cycled spontaneously. These values depend on various factors and should be interpreted carefully. For example, the percentage of triggered breaths can be overestimated with auto-triggering and may not account for ineffective efforts or unintentional leaks. The percentage of spontaneously cycled breaths is influenced by cycling criteria settings, inspiratory time range and unintentional leaks. A detailed analysis involves interpreting pressure and flow waveforms over a specific time axis, like 1 minute per epoch. This helps to identify phase asynchronies (ineffective efforts, auto-triggering, premature cycling, double triggering and delayed cycling) and flow asynchronies (flow overshoot or insufficient flow).
Nocturnal pulse oximetry is a simple, cost-effective screening tool for assessing NIV’s impact on gas exchanges. Nocturnal pulse oximetry, whether standalone or connected to a ventilator, provides visual examination of SpO2, leaks, and waveforms. It is suitable for detecting rapid desaturation during upper airway obstructions. While not recommended for certain populations, it can screen for respiratory events, predict outcomes and monitor night-time NIV use. Interpreting nocturnal pulse oximetry requires at least 4.5 hours of sleep recording with minimal artefacts, excluding unintentional leaks. Visual inspection complements statistics due to limitations. Abnormal results may prompt ventilator adjustments.
Mechanical ventilation FAQ
Non-invasive ventilation (NIV) refers to any type of ventilation that is delivered through a non-invasive interface like a nasal mask, full-face mask or mouthpiece. As technology improves, non-invasive ventilation is becoming an increasingly popular way of delivering mechanical ventilation. Non-invasive ventilation can provide effective ventilation without the need for intubation or tracheostomy. This makes NIV easier to implement and more comfortable for the patient and lowers the risk of infection compared to invasive methods. NIV offers more flexibility to non-dependent patients as ventilation can be intermittent. For example, they can receive treatment only during the night, can remain outside intensive care units, and can be more easily treated in their home.
Invasive ventilation (IV) is usually used in patients who fail non-invasive ventilation (NIV). It is sometimes used when a patient has acute respiratory failure or is dependent on long-term home ventilation. With a tracheostomy tube in place, leaks can be controlled and ventilation assured. For patients with excessive secretions, the tracheostomy provides direct access for secretion removal through suctioning. IV has a higher complication rate than NIV. Patients may find it uncomfortable and it can affect their ability to talk and swallow. IV is also associated with higher infection rates and with secretions.
Mechanical ventilation, whether invasive or non-invasive, delivers air to inflate the lungs, almost in the way that a person blows air to inflate a balloon. It does this by delivering air at a pre-set pressure (barometric ventilation) or a pre-set volume (volumetric ventilation) during the inspiration phase of the patient’s breathing cycle.
Barometric ventilation delivers a pre-set pressure with each inspiration, but the patient’s tidal volume and flow rate are not fixed and can vary with each breath. Bilevel ventilators typically provide barometric ventilation and use a leak circuit. They are primarily used for non-invasive ventilation (NIV), although some can be used for non-dependent, invasively ventilated patients.
Volumetric ventilation delivers a pre-set volume of air over the inspiratory period. The pressure needed to deliver this volume varies and the flow rate can be adjusted.
Hybrid modes combine aspects of both volumetric and barometric ventilation. This ensures that the volume of airway pressure that is delivered is continuously adjusted to achieve the pre-set volume.
Typically, invasive ventilation (IV) is provided through a ventilator which can deliver high pressures, monitor exhaled volumes, and offer a wide range of alarms.
Ventilators can deliver ventilatory support through a leak circuit or a valve circuit.
A leak circuit is a single circuit that has a deliberate leak built into it. This leak can be in the circuit itself or in the interface mask. As the patient breathes out, the exhaled air exits through the leak. For this reason, devices used with a leak circuit must always have a flow of air going through the circuit in order to wash out the exhaled air.
A non-intentional leak is a primary cause of patient-ventilator asynchrony. Barometric ventilators, however, are very good at compensating for the variable and non-intentional leaks that are inherent to NIV.
Valve circuits have an active inhalation and exhalation valve which opens and closes with inspiration and expiration. Valve circuits can be used in both IV and NIV ventilation, in barometric, volumetric and mixed modes. Valve circuits can be used in either single- or double-limb configuration. Non-vented masks must be used for non-invasive valve ventilation. The double-limb circuit is often used for patients who need their exhalation volume closely monitored, such as very young patients or those with an advanced stable condition. Valve circuits are usually the circuit of choice for invasively ventilated patients, but they can also be used non-invasively in barometric and, in some cases, volumetric modes.
Management of respiratory diseases

Managing COPD
International guidelines recommend NIV for stable hypercapnic COPD patients as it can improve survival and quality of life and reduce the risk of hospital admission.

Managing OHS
NIV may be recommended for patients experiencing hypoventilation with mild to no OSA, those with comorbid pulmonary hypertension, and individuals who do not respond to CPAP.

Managing NMD
Nocturnal NIV can improve gas exchange, sleep, symptoms and survival for patients with NMD. Diurnal NIV may also be required for those with progressive disease.
Research on home non-invasive ventilation
Explore significant insights from recent clinical research and understand their implications for making informed treatment decisions and selecting appropriate patients.
This content is intended for health professionals only.
Please refer to the user and clinical guides for relevant information related to any contraindications, warnings and precautions to be considered before and during use of the products.
References:
- M.L. Duiverman, J.M. Vonk, G. Bladder, J.P. van Melle, J. Nieuwenhuis, A. Hazenberg, et al.
Home initiation of chronic non-invasive ventilation in COPD patients with chronic hypercapnic respiratory failure: a randomised controlled trial. Thorax, 75 (2020), pp. 244-252 - R.J.M. van den Biggelaar, A. Hazenberg, N.A.M. Cobben, M.A. Gaytant, K.M. Vermeulen, P.J. Wijkstra.
“A randomized trial of initiation of chronic non-invasive mechanical ventilation at home vs in-hospital in patients with Neuromuscular Disease and thoracic cage disorder”: The Dutch Homerun Trial.Chest, (2020),
http://dx.doi.org/10.1016/j.chest.2020.07.007 - A. Hazenberg, H.A. Kerstjens, S.C. Prins, K.M. Vermeulen, P.J. Wijkstra.
Initiation of home mechanical ventilation at home: a randomised controlled trial of efficacy, feasibility and costs.
Respir Med., 108 (2014), pp. 1387-1395
http://dx.doi.org/10.1016/j.rmed.2014.07.008 | Medline - E. Bertella, P. Banfi, M. Paneroni, S. Grilli, L. Bianchi, E. Volpato, et al.
Early initiation of night-time NIV in an outpatient setting: a randomized non-inferiority study in ALS patients.
Eur J Phys Rehabil Med., 53 (2017), pp. 892-899
http://dx.doi.org/10.23736/S1973-9087.17.04511-7 - Duiverman ML. “Tricks and tips for home mechanical ventilation” Home mechanical ventilation: set-up and monitoring protocols. Pulmonology. 2021 Mar-Apr;27(2):144-150. doi: 10.1016/j.pulmoe.2020.08.002. Epub 2020 Sep 8. PMID: 32912752.
- Arnal JM, Thevenin CP, Couzinou B, Texereau J, Garnero A. Setting up home noninvasive ventilation. Chron Respir Dis. 2019 Jan-Dec;16:1479973119844090. doi: 10.1177/1479973119844090
- Cruz J, Brooks D, Marques A. Home telemonitoring effectiveness in COPD: a systematic review. Int J Clin Pract 2014; 68(3): 369-78.
- Arnal JM, Oranger M, Gonzalez-Bermejo J. Monitoring Systems in Home Ventilation. J Clin Med. 2023 Mar 10;12(6):2163. doi: 10.3390/jcm12062163.
- Jiang W, Jin X, Du C, Gu W, Gao X, Zhou C, Tu C, Chen H, Li H, Shen Y, Zhang Y, Ge X, Sun Y, Zhou L, Yu S, Zhao K, Cheng Q, Zhu X, Liao H, Bai C, Song Y. Internet of things-based management versus standard management of home noninvasive ventilation in COPD patients with hypercapnic chronic respiratory failure: a multicentre randomized controlled non-inferiority trial. EClinicalMedicine. 2024 Mar 10;70:102518. doi: 10.1016/j.eclinm.2024.102518.
Last update: 19.06.24