Research in home high flow therapy for COPD
Discover key findings from recent clinical research on the mechanisms of action of home high-flow therapy (HFT), and the clinical outcomes in patients with COPD.
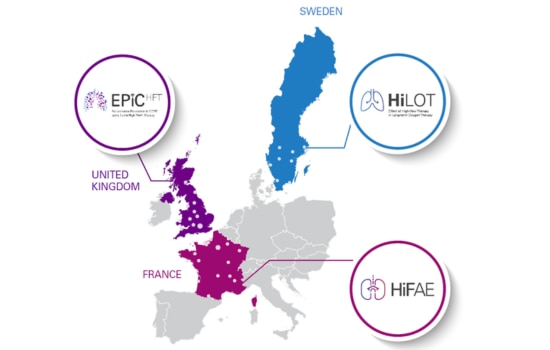
Home HFT studies progressing in Europe
There are currently three key studies taking place in centres across France, Sweden and the UK – our infographic provides a quick overview, with more detail on each study available below.
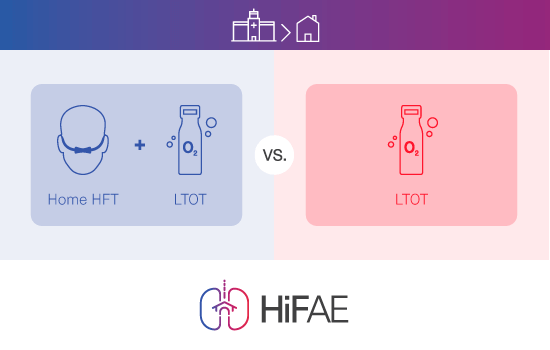
The HiFAE trial
HiFAE (home high-flow therapy with oxygen to reduce acute exacerbations of COPD) is a randomised, controlled trial designed to evaluate the efficacy of home high-flow therapy with oxygen, versus standard long-term oxygen therapy (LTOT) in patients with COPD. This ongoing study is being conducted at 18 centres in France (N=406). The primary endpoint is the time to first hospital admission for acute exacerbation of COPD (AECOPD) or death.
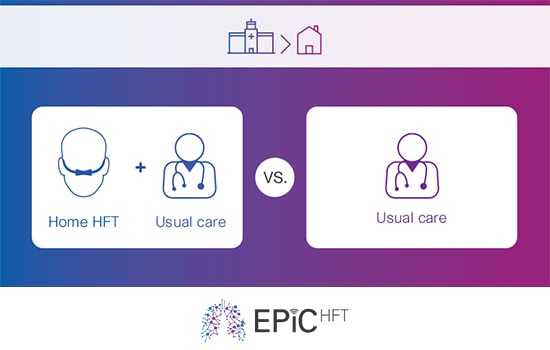
The EPIC-HFT Trial
EPiC-HFT (exacerbation prevention in COPD using home high-flow therapy) is a randomised, controlled trial investigating the effect of home high-flow therapy (HFT) as an adjunct to usual medical care on admission-free survival following a severe exacerbation of COPD . This ongoing study is being conducted at 14 centres in the UK (N=502) and the primary endpoint is 12-month all-cause admission-free survival.
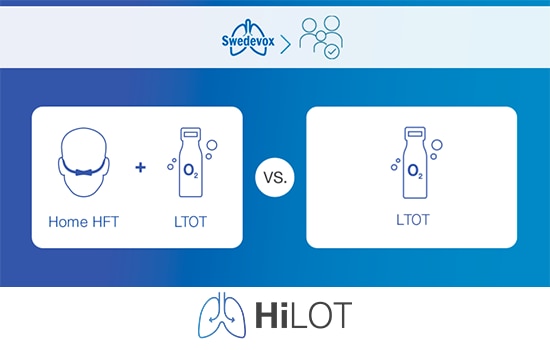
The HiLOT Trial
HiLOT (Effect of High-flow therapy in Long-term Oxygen Therapy) is a registry-based, randomised controlled trial of the effect of using home high-flow therapy (HFT) with long-term oxygen therapy (LTOT) during one year in people with COPD or ILD, vs using LTOT alone. This ongoing study is being conducted at 10 centres in Sweden (N=310 (270 COPD patients and 40 ILD patients)). The primary endpoint is time to first hospitalisation or all-cause death in the year following randomisation in COPD patients.
HFT is simple and easy-to-operate and delivers both clinical and patient outcome benefits in domiciliary use for COPD. HFT is currently used in the acute hospital setting in adults and is emerging as an option for long-term home use in COPD patients. 6,7
Mechanisms of action and clinical benefits
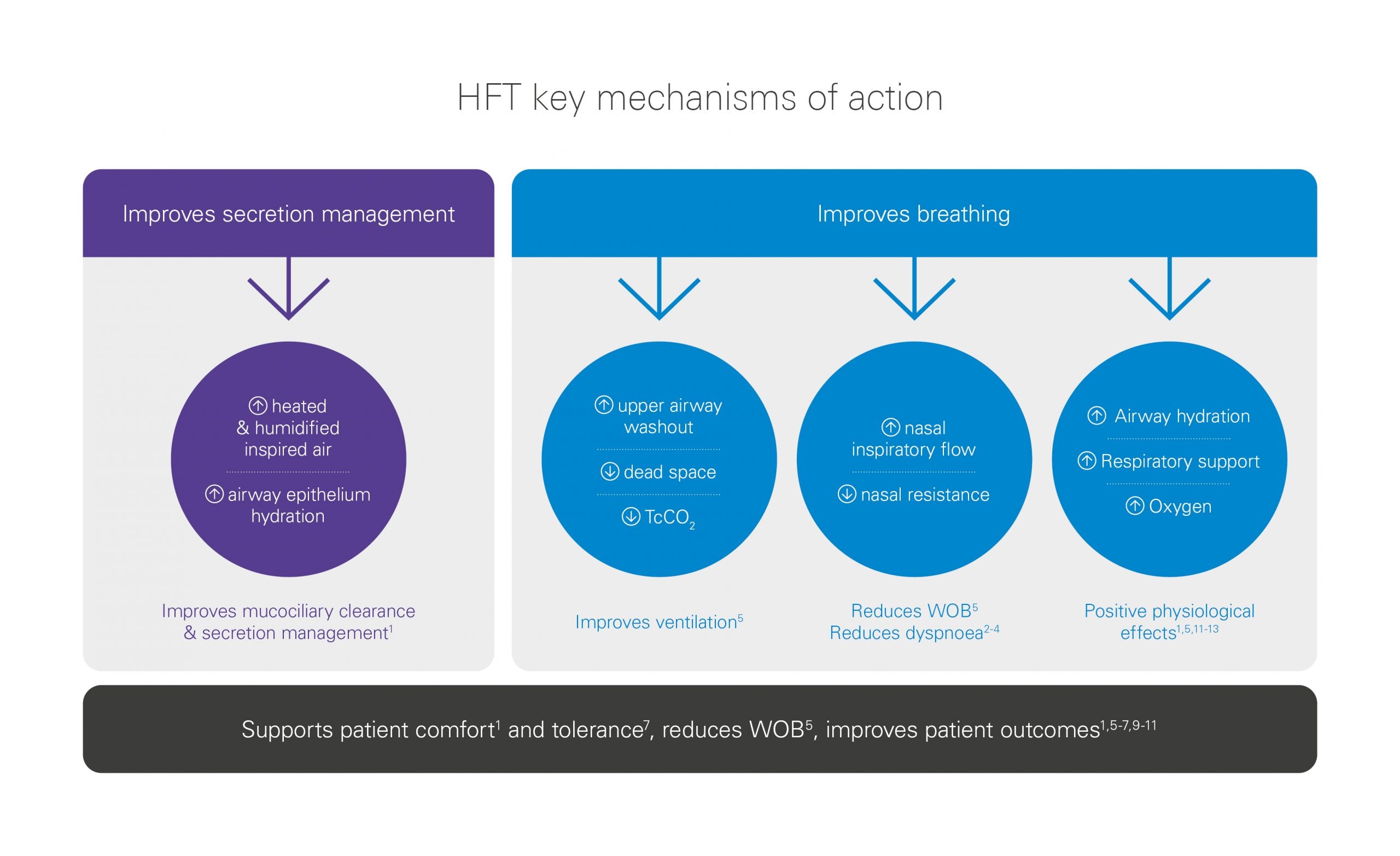
HFT works via multiple mechanisms including mucociliary clearance and secretion management, and improved respiratory mechanics which reduce WOB and improves patient comfort.1,5,11,12,13
Outcomes and patient benefits
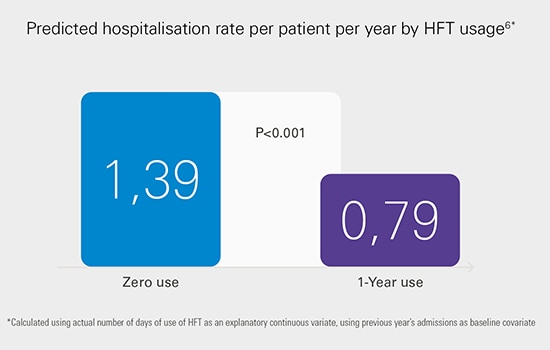
Adjunctive home HFT can reduce acute exacerbation and hospitalisation rates in COPD patients,6,7 and improve symptoms such as mucus retention1, cough1 and dyspnoea during high intensity exercise, 2-4 while maintaining or improving patient QoL vs usual care. 6,7
Patient comfort and quality of life

Patients with COPD receiving long-term HFT at home have shown preserved or improved QoL scores vs those receiving usual care, including LTOT alone.6,7 HFT also seems to be well tolerated by patients7 and supports patient comfort by improving mucociliary clearance and secretion management1 and reducing dyspnoea during high intensity exercise. 2-4
High-flow therapy at home: a patient case study
What effect did home HFT have on a 64-year-old ex-smoker with COPD GOLD 3D?
Respiratory specialist Dr Díaz Lobato presents a detailed case study alongside evidence from recent research.
This content is intended for health professionals only.
References:
- Hasani A, et al. Domiciliary humidification improves lung mucociliary clearance in patients with bronchiectasis. Chron Respir Dis 2008;5:81-86.
- Cirio S, Piran M, Vitacca M, Piaggi G, Ceriana P, Prazzoli M, et al. Effects of heated and humidified high flow gases during high-intensity constant-load exercise on severe COPD patients with ventilatory limitation. Respiratory Medicine 2016;118:128–32.
- Neunhäuserer D, Steidle-Kloc E, Weiss G, Kaiser B, Niederseer D, Hartl S, et al. Supplemental Oxygen During High-Intensity Exercise Training in Nonhypoxemic Chronic Obstructive Pulmonary Disease. The American Journal of Medicine 2016;129(11):1185–93.
- Chatila W, Nugent T, Vance G, Gaughan J, Criner GJ. The Effects of High-Flow vs Low-Flow Oxygen on Exercise in Advanced Obstructive Airways Disease. Chest 2004;126(4):1108–15.
- Fraser JF, et al. Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax 2016;71:759-761.
- Storgaard LH, et al. Long-term effects of oxygen-enriched high-flow nasal cannula treatment in COPD patients with chronic hypoxemic respiratory failure. Int J Chron Obstruct Pulmon Dis 2018;13:1195-1205.
- Rea H, et al. The clinical utility of long-term humidification therapy in chronic airway disease. Respir Med 2010;104:525-533.
- Nagata K, Kikuchi T, Horie T, Shiraki A, Kitajima T, Kadowaki T, et al. Domiciliary High-Flow Nasal Cannula Oxygen Therapy for Stable Hypercapnic COPD Patients: A Multicenter, Randomized Crossover Trial. Annals of the American Thoracic Society. 2017.
- Elshof J, Duiverman ML. Clinical Evidence of Nasal High-Flow Therapy in Chronic Obstructive Pulmonary Disease Patients. Respiration 2020;99:140-153.
- Nishimura M. High-Flow Nasal Cannula Oxygen Therapy in Adults: Physiological Benefits, Indication, Clinical Benefits, and Adverse Effects. Respir Care 2016;61:529-541.
- Vogelsinger H, et al. Efficacy and safety of nasal high-flow oxygen in COPD patients. BMC Pulm Med 2017;17:143.
- Biselli P, Fricke K, Grote L, Braun AT, Kirkness J, Smith P, et al. Reductions in dead space ventilation with Nasal High Flow depend on physiologic dead space volume – Metabolic hood measurements during sleep in patients with COPD and controls. European Respiratory Journal. 2018.
- McKinstry S, Pilcher J, Bardsley G, Berry J, Van de Hei S, Braithwaite I, et al. Nasal high flow therapy and PtCO2 in stable COPD: A randomized controlled cross-over trial. Respirology. 2017.
Content last updated: 06/2024